Gut Testing and the GI Map
Feb 03, 2026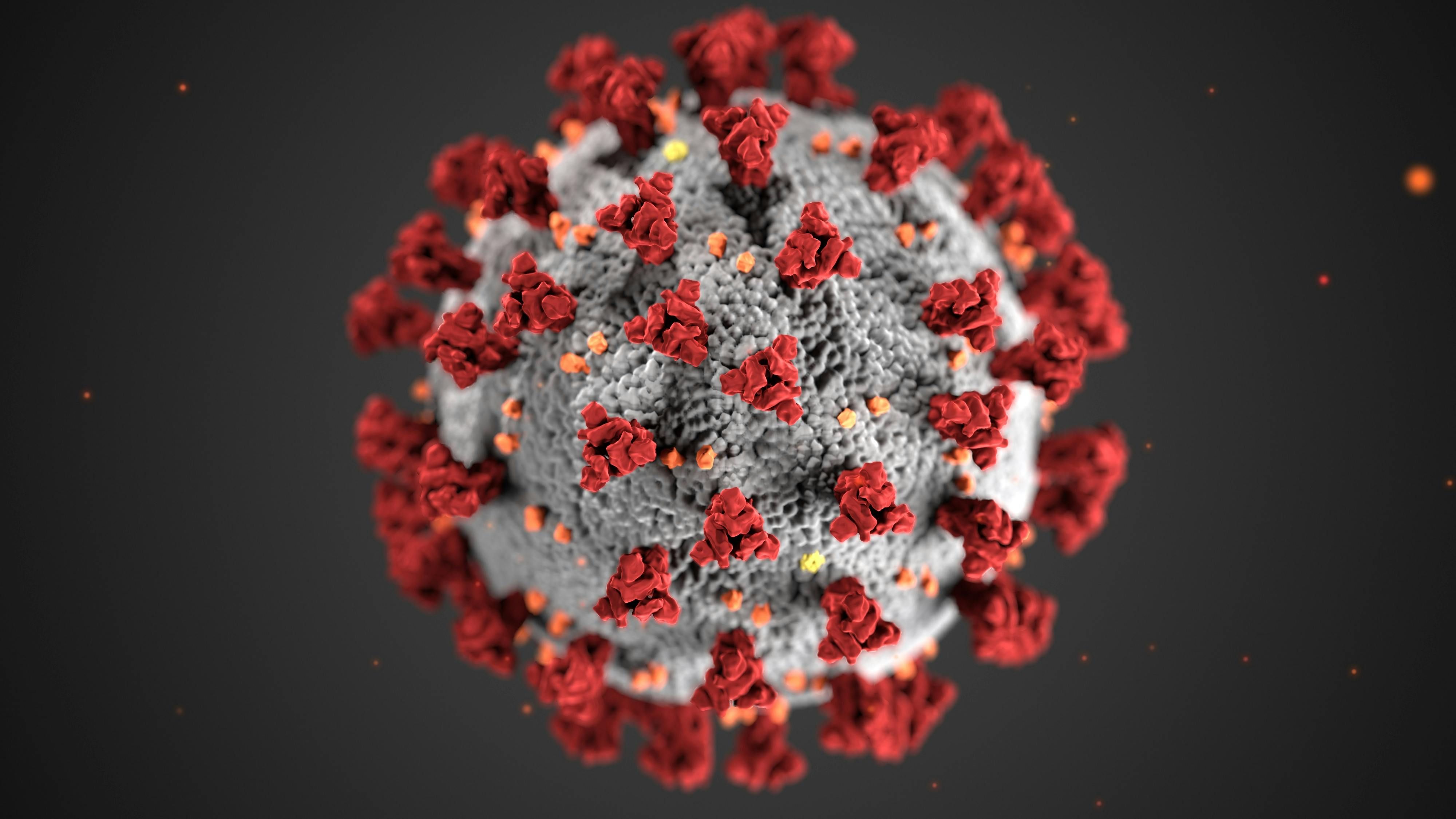
Gut testing has become an important tool for understanding health beyond basic symptoms and routine lab work. Many people struggle with digestive issues, fatigue, skin problems, autoimmune conditions, or chronic inflammation for years without clear answers. Because the gut plays a central role in digestion, immune regulation, hormone balance, and nutrient absorption, testing the gastrointestinal system can reveal underlying patterns that are easy to miss with standard blood tests or imaging.
Traditional gut testing has often focused on identifying acute infections or obvious abnormalities. While this approach is useful in certain situations, it does not always explain chronic or complex symptoms. Functional gut testing looks deeper by evaluating how well the digestive system is working, how balanced the gut microbiome is, and how the immune system is responding within the gut. This broader view allows providers to connect digestive health to whole body symptoms.
One of the most commonly used functional gut tests is the GI MAP test. GI MAP stands for Gastrointestinal Microbial Assay Plus and it uses DNA based technology to identify and quantify microbes in the stool. Instead of relying on culture methods, which can miss many organisms, this test detects microbial DNA using quantitative PCR. This makes it possible to identify bacteria, parasites, viruses, and fungi with a high degree of sensitivity.
A major focus of gut testing, including the GI MAP, is the gut microbiome. The microbiome is the ecosystem of bacteria living in the digestive tract that influences digestion, immune signaling, inflammation, and even brain function. An imbalance in this ecosystem, known as dysbiosis, may contribute to symptoms such as bloating, constipation, diarrhea, food sensitivities, anxiety, and autoimmune flares. Gut testing helps determine whether beneficial bacteria are low, opportunistic organisms are overgrown, or pathogenic microbes are present.
Beyond microbes, comprehensive gut testing evaluates digestive and inflammatory markers. These markers offer insight into how effectively food is being broken down and absorbed, as well as whether the gut lining is under immune stress. Elevated inflammatory markers may suggest irritation, infection, or increased intestinal permeability. Low digestive markers can point to enzyme insufficiency or impaired nutrient absorption, even in individuals eating a well balanced diet.
Another benefit of advanced gut testing is its ability to identify low grade or chronic infections that may not cause obvious illness but still affect health over time. Some organisms can quietly disrupt the gut environment, strain the immune system, and contribute to systemic symptoms. Identifying these patterns allows for targeted and individualized treatment rather than guessing or using broad approaches.
It is important to understand that gut test results should never be interpreted on their own. Symptoms, medical history, diet, stress levels, and lifestyle factors all influence how results are understood. Not every abnormal marker requires treatment, and not every normal value means the gut is functioning optimally. Skilled interpretation is essential to avoid unnecessary interventions and to focus on what truly matters for the individual.
Gut testing is not about labeling disease but about gaining insight. Tests like the GI MAP help shift care from symptom management to root cause exploration. When used appropriately, gut testing can guide personalized nutrition, supplementation, and lifestyle strategies that support long term digestive and overall health.
